
Please click here for a history of Wegener’s
Wegener’s Granulomatosis (GPA or Granulomatosis with polyangiitis) is a rare condition of unknown cause that develops as a result of inflammation in the blood vessels. Around 500 people are diagnosed with the condition each year in the UK. It can occur at any age but is most often seen in middle age (the 4th and 5th decade) and distributed equally between men and women. It is highly unusual for it to occur in two people in the same family, so there is not a strong genetic link. As all parts of the body have blood vessels within them it can affect many different organs and systems including the sinuses, ears, throat, lungs, kidneys, nerves, brain and skin. Joint pains and eye symptoms can also occur. Less often the heart and bowels can become involved and some patients seem to be at a greater risk of developing blood clots in the leg or lung.
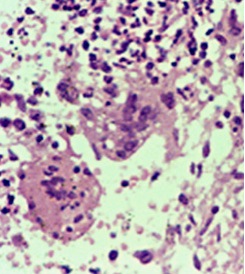
Inflammation in the blood vessels occurs as the immune system, which usually works to fight infection, begins to attack your body. This is termed autoimmunity. The steps that lead to this occurring are not clearly understood. GPA is caused by a particular type of inflammation which has an easily recognisable pattern when tissues are examined under a microscope. This is a result of white blood cells arranging themselves in a certain way called a granuloma, pictured below:
The Symptoms
What symptoms can you experience when the condition first develops?
Early in the disorder, symptoms are usually very non-specific and include a general feeling of being unwell, flu-like symptoms, loss of appetite, fevers, night sweats, severe fatigue and weight loss. The most common symptoms include sinusitis, a persistent runny nose, nose bleeds, mouth or nose ulcers, a persistent cough, painful joints and muscles or skin rashes. Other common symptoms are hoarseness, noisy breathing, earache, hearing loss, recurrent ear infections and discharge from the ears. Patients may also experience shortness of breath or chest pain, and some people may cough up blood. The symptoms that an individual experiences depend on which blood vessels are inflamed and can vary greatly. For example if the blood vessels in the skin are inflamed then skin rashes will be seen and if the blood vessels in the eyes or brain are affected then you may develop painful red eyes, headaches and heaviness or weakness in the arms and legs.
How is the diagnosis made?
A group of expert doctors have put together a list of typical features that should be expected to be present when making a diagnosis of GPA. In reality these do not always apply as each individual case tends to be unique and the diagnosis should be made by a trained specialist.
The presence of 2 of the following 4 findings is usually necessary for a specialist to consider the diagnosis of GPA.
- Nose or mouth inflammation (painful or painless oral ulcers or purulent or bloody nasal discharge)
- Abnormal chest x-ray showing nodules, shadows, or cavities
- Abnormal urinary tests (Blood in the urine when tested with a dipstick or broken up blood cells seen under a microscope)
- Granulomatous inflammation (the typical white blood cell pattern seen under a microscope) on biopsy of an artery or area around a blood vessel.
The ANCA blood test is also used to make the diagnosis.
Chest x-ray of a patient with a flare of GPA showing the typical cavitating lung nodules

CT chest of the same patient illustrating the value of CT in defining the nodules
What tests might you expect your doctor to conduct?
Patients with generalised symptoms described above will need a full history and a thorough physical examination. You can help your doctor by trying to give as full an account of your symptoms as possible.
Routine laboratory tests — Blood count, kidney and liver tests and levels of blood inflammation such as the CRP (C-reactive Protein) and ESR. The urine should be tested for the presence of blood and protein.
Antineutrophil cytoplasmic antibodies — The ANCA test
Approximately 90 to 95 percent of patients with generalised GPA have a positive ANCA test. In cases with more limited involvement, for example just the sinuses and ears, up to 40 percent of patients may have a negative ANCA test, which can be misleading.
Tissue biopsy — Depending on the areas affected by GPA and your doctor’s concern about making sure there isn’t another problem, for example infection, you may need to have a biopsy. These can be taken from the skin and nose and sometimes from the lungs or kidneys. The tissue usually shows the typical features of inflammation and granulomas when examined under the microscope but this is not always the case.
X-rays and other tests – Your doctor will decide which x-rays and other tests need to be done depending on the areas affected by GPA. You may need a chest x-ray or scan of the chest or abdomen.
Please click here for the A4 Wegener’s Trust leaflet
Please click here for the abstract of our published paper on diagnosis and classification of GPA
